3 Chapter 3
LAB 3
Introduction to the Cardiovascular System
Prepared by Jason R. Jones, University of North Alabama
OBJECTIVES
After completing these laboratory activities, you should understand/be able to:
- Define cardiovascular system and be able to describe the main parts and functions of the cardiovascular system.
- Identify the chambers, valves, and major vessels of the heart
- Define the following types of blood vessels: arteries, arterioles, capillaries, venules, veins
- Identify some of the major vessels carrying blood to (arteries) and carrying blood away from (veins) major body regions
- The difference between systemic circulation and pulmonary circulation, and be able to trace the path of blood through the heart in each
- How heart rate is measured, and how various factors can influence heart rate
- The typical healthy range of human heart rate
- The concept of blood pressure, including the difference between systolic and diastolic pressure
- How systolic and diastolic pressures are measured, and how these values are reported in a blood pressure reading
- The importance of blood pressure as a measure of health, and know the maximum values of a healthy blood pressure reading
- Define the terms atherosclerosis, coronary arteries, coronary bypass surgery, myocardial infarction, plaque, stent
INTRODUCTION
The cardiovascular system serves as the primary means of transporting molecules throughout the body to the trillions of cells that require a supply of nutrients/oxygen for the required constant production of ATP and our survival. Additionally, our cells’ metabolism produces toxic or unusable wastes that must be removed.
The cardiovascular system (cardio- means “heart”, and vascular means “vessels or tubes”) consists of the heart (“pumping station”) and the blood vessels (arteries, arterioles, veins, venules, and capillaries), which can be thought of as highways along which the blood moves.
ACTIVITY I: Anatomy of the Heart
The heart is a located in the thoracic cavity of the body, along with the lungs. It is situated on the midline of the body, behind and slightly to the left of the sternum, which protects it. Look at the provided human heart model and the heart in the human torso model. Externally, several structures of the heart are visible from an anterior (front view). First, you should note the apex, or tip of the heart, which points downwards and towards the left side of the body. You should also notice two earlike flaps towards the base (top) of the heart. These flaps are called the auricles, and are part of the upper chambers of the heart, which we will discuss below. You will also notice several large blood vessels connected to the heart, namely the large, arching aorta, which is the largest artery in the body, the pulmonary artery or pulmonary trunk, which branches into the left and right pulmonary arteries (only the left pulmonary artery can be seen in the anterior view), the superior vena cava, and the right pulmonary veins. Use Figures 1 and 2 on the following page to help you identify the structures in bold text on the provided heart model. There will be a worksheet at the end of this lab exercise, where you will also need to identify these specific structures on the heart model that your instructor may take up after lab, so be sure to fill these in, as well.

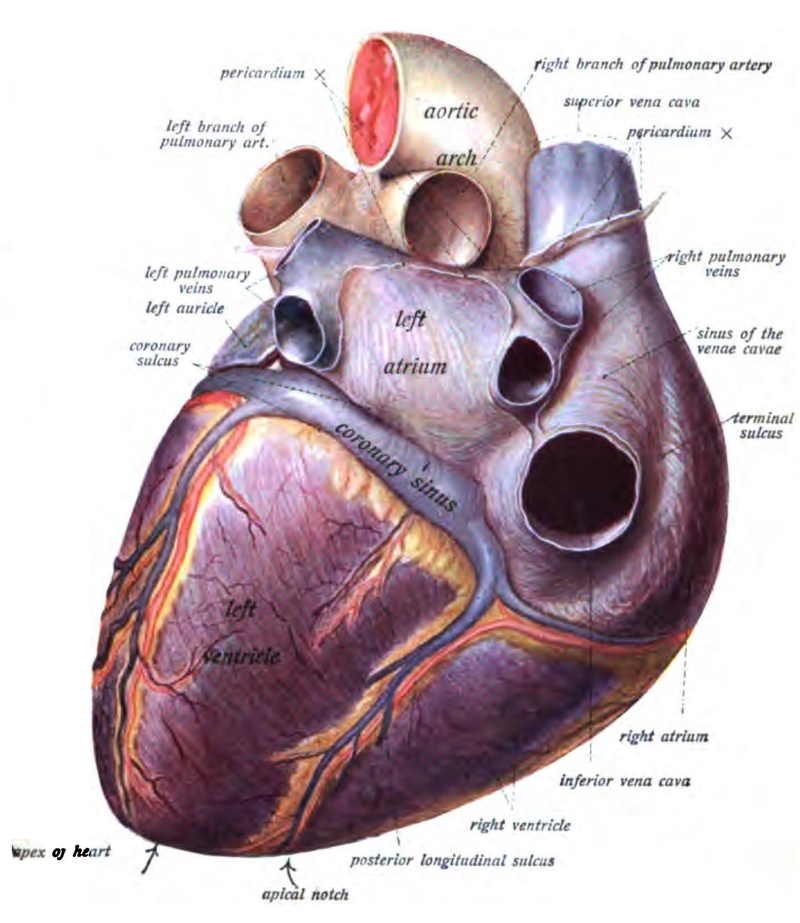
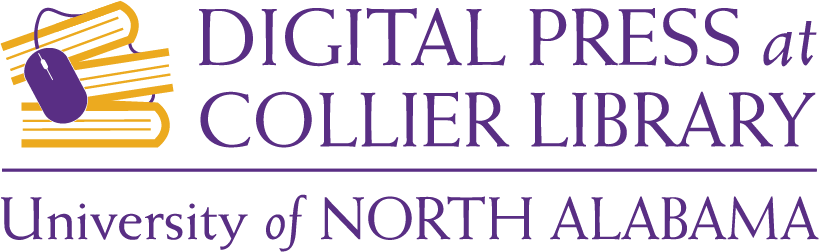
Figure 1. Heart external anatomy, anterior view.Figure 2. Heart external anatomy, posterior view.
Now observe the external anatomy of the heart from the posterior view. From the posterior view, the aorta is still visible, as is the superior vena cava. However, on the posterior side of the heart, you can now observe the right pulmonary artery (which branches from the pulmonary trunk), the right pulmonary veins, and the inferior vena cava. We will discuss these major blood vessels in greater detail below. In both views of the heart, you can also see several smaller blood vessels covering the surface of the heart. These are the coronary arteries and cardiac veins, and serve as a blood supply for the tissues of the heart itself.
Now remove the front portion of the human heart model, and notice that internally, the heart is divided into several chambers. Mammals (including ourselves), have a heart that is divided into four chambers: two upper chambers called the atria (left atrium and right atrium), and two lower chambers called the ventricles (left ventricle and right ventricle). We can describe the functions of these chambers in two different ways. In one way, we can think about the differences between the upper chambers (atria) and the lower chambers (ventricles). You can think about the atria as the receiving chambers of the heart, as the atria receive blood from other parts of the body. One way to remember this is to think about the atrium of a building, which is usually the receiving area of the building. The lower chambers, or ventricles, have the main function of distributing blood elsewhere in the body. Another way to remember that the ventricles are the lower chambers of the heart is to look at the apex, or lower tip of the heart, which has a V-like shape. Examine Figure 3 on the following page, and use it to help you identify the structures in bold text on the provided heart model. There will be a worksheet at the end of this lab exercise, where you will also need to identify these specific structures on the heart model that your instructor may take up after lab, so be sure to fill these in, as well.
Figure 3. Heart internal anatomy, anterior view.
Notice that the heart is separated into left and right sides by a thick muscular wall called the septum, which separates the circulation of oxygenated and deoxygenated blood. This means that the circulation of blood in our bodies is actually separated into two different pathways, or circuits: the systemic circuit and the pulmonary circuit. The pulmonary circuit consists of the pathway of deoxygenated blood from the heart to the lungs for re-oxygenation, and then back to the heart. The systemic circuit consists of the pathway of oxygenated blood from the heart to all of the rest of the body (where cells deplete the oxygen supply in the blood), and back to the heart. We’ll look at each of these circuits in more detail later, but first, let’s continue examining the basic anatomy of the mammalian heart.
Another major feature seen in the mammalian heart is the presence of four special valves, all of which can be seen in Figure 3. These valves are very important, because their main function is to ensure that the flow of blood through the heart is only in a single direction. There are two main kinds of valves that are seen in the heart: atrioventricular valves and semilunar valves.
There are two atrioventricular valves, which separate the atrium from the ventricle on each side of the heart. If you look closely at each of the AV valves in the heart model, you will see that each of them are made up of several leaflets, or flaps. The right AV valve consists of three of these leaflets and is referred to as the tricuspid valve. The left AV valve consists of two of these leaflets, and referred to as the bicuspid valve. More commonly, however, the left AV valve is often called the mitral valve. The atrioventricular valves ensure that blood only flows from atrium to ventricle, and not the other way around. When the atria contract, the increased pressure of blood in the atria forces the AV valves open, and blood then flows into the ventricles. However, when the ventricles contract, the AV valves prevent blood from flowing back into the atria. This is achieved due to the unique structure of the AV valves themselves. Notice that at the bottom of each of the AV valves, they are connected to the walls of the ventricles by long, thin, cordlike tendons called the chordae tendineae. When the ventricles contract, the increase in blood pressure in the ventricles could potentially force the AV valves to open in the wrong direction. However, tension provided by the chordae tendineae prevents this from happening.
There are also two semilunar valves in the heart, which separate the ventricles from the main blood vessels they supply. Between the left ventricle and the aorta is the aortic semilunar valve, and between the right ventricle and the pulmonary trunk, there is the pulmonary semilunar valve. The semilunar valves ensure that blood flows only in the direction of ventricle to vessel, and not the other way around. When the ventricles contract, the increased pressure of blood in the ventricles forces the semilunar valves open, causing blood to flow into the major vessels supplied by each ventricle. However, due to the force of gravity, blood has a tendency to flow downward, back towards the ventricles. However, the structure of the semilunar valves prevents this. Each semilunar valve is made up of three cuplike structures. When the ventricles contract, imagine the pressure of blood from the ventricles, forcing those cups upward and onto their sides, opening the semilunar valves. However, as the ventricles relax, as blood begins to flow downwards back towards the ventricles, that blood fills those cups up, causing them to tip back upright, closing the valves.
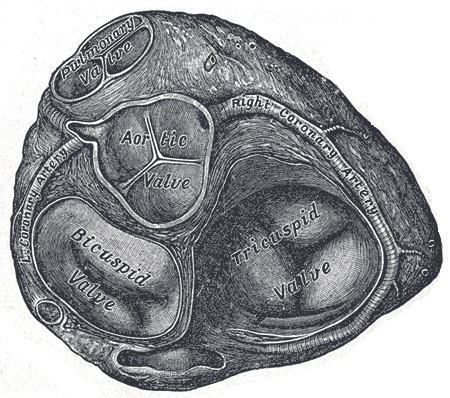
Figure 4. View of valves in the heart (cross section)
**What are the two major circuits of the heart, what is the function of each circuit?**
a. ______________________ a. Function:_______________________________
b.______________________ b. Function:_______________________________
ACTIVITY II: Anatomy of Blood Vessels
The heart acts as the pump that provides the force to deliver blood (and materials therein). The blood vessels are the pathways through which blood is delivered to locations throughout the body. The five major types of blood vessels in the cardiovascular system are: arteries, arterioles, venules,veins, and capillaries. Arteries and arterioles are blood vessels that carry blood in a direction away from the heart; arterioles are smaller branches of larger arteries. Veins and venules are blood vessels that carry blood in a direction back towards the heart; venules are smaller branches of larger veins. Capillaries are the smallest blood vessels where exchange of materials (water, gases, nutrients) occurs between blood and tissues.
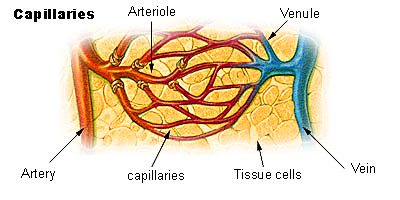
Figure 5. Comparative sizes of blood vessel types.
Aside from the difference in the direction in which they carry blood, arteries and veins have some anatomical differences, as well. Examine Figure 6 . Notice that the walls of arteries are thicker and much more muscular than the walls of veins. If you think about the fact that arteries are carrying blood away from the heart, this should make sense. Blood being carried away from the heart is moved as a result of the strong pumping force of the heart, is under higher pressure, and arteries need much thicker walls to withstand pressure without rupturing.
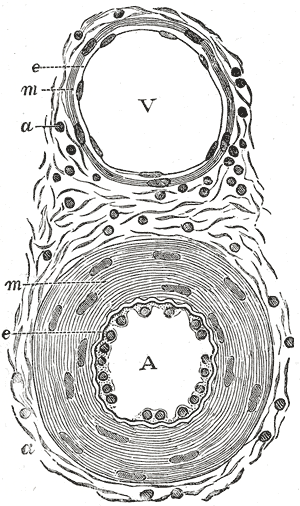
Figure 6. Comparison of veins & arteries. V = vein, A = artery, e = endothelium (simple squamous epithelial tissue), m = tunica media (mostly smooth muscle), a = tunica adventitia (connective tissue)
The blood flowing through veins is under lower pressure and as a result, veins have thinner walls and larger lumens (openings). This is an advantageous, because it allows for greater blood flow with less resistance from surrounding layers of their walls, facilitating movement of blood back towards the heart. Finally, veins possess valves, while arteries do not. Figure 7, shows valves in veinsthat ensure one-way flow of blood (towards the heart). However, think for a minute about the blood in your legs, for example. If that blood has to get back to the heart, it has to move upwards, against the force of gravity. How is that accomplished? The valves in veins are part of this answer, but the musculoskeletal system also plays an important part in this role.
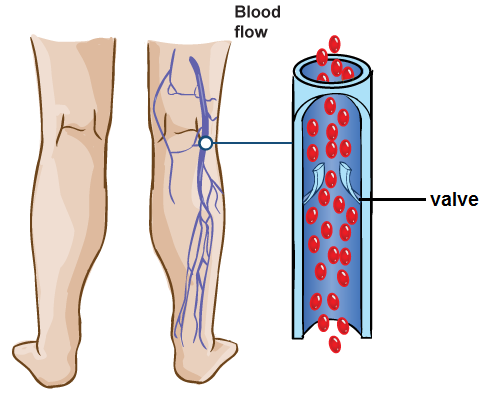
Figure 7. Illustration of how valves in veins prevent backflow of blood due to gravity (image courtesy of the U.S. National Library of Medicine).
When we walk and move around, contractions of our skeletal muscles puts pressure on our veins, like those in our legs, for example. That pressure forces blood to move through our veins. The valves in these veins only allow that movement in one direction. The structure of the valves prevent backflow of blood back down into the legs. Due to gravity, the blood in our legs has a natural tendency to flow downward, but as it does so, that closes the valves in those veins, similar to the way that the semilunar valves work in the heart.
Capillaries are very different than both arteries and veins. Capillaries are the smallest blood vessels, and are so thin, they only allow red blood cells to pass through them in single file. They are only made up of a single layer, the endothelium, which is simple squamous epithelial tissue. This property is what makes capillaries able to fulfill their role of exchange of materials (water, gases, nutrients, hormones, and wastes) between blood and tissues. Since the walls of capillaries are only a single layer thick, that makes it really easy for some molecules (water, oxygen, and carbon dioxide) to diffuse directly across their walls. Additionally, there are also tiny slits or pores between the endothelial cells, which allow molecules or cells that are small enough to fit through them to move into or out of the capillary. This also comes in handy in the case of infection in a particular tissue, because white blood cells, which are part of the immune system’s arsenal against invaders, are small enough to move through these slits and into the infected tissue.
Now that we’ve discussed the basic anatomy of blood vessels, let’s examine some of the major blood vessels that supply or drain various regions of the body. Examine Figure 8 on the following page, and use that figure to match various blood vessels in the figure to their appropriate descriptions on the worksheet at the end of this lab exercise.
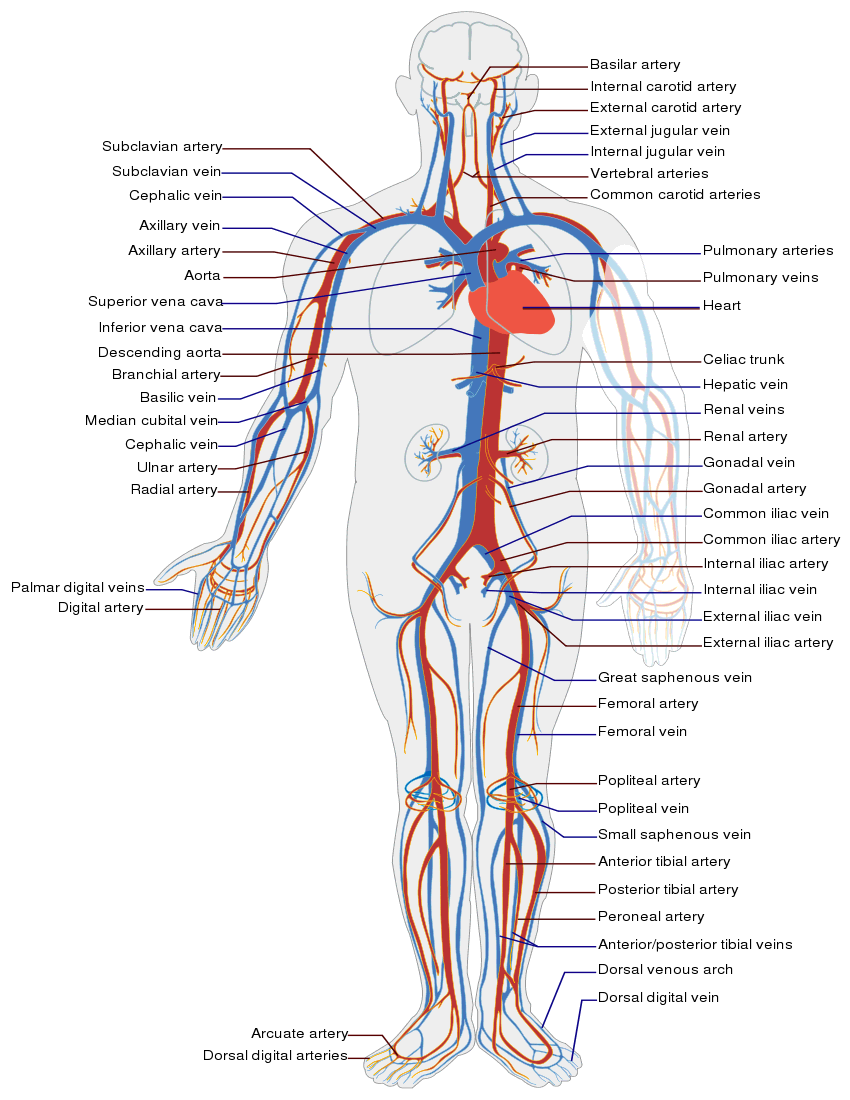
Figure 8. Major arteries and veins of the cardiovascular system.
ACTIVITY III: Pulmonary and Systemic Circulation
Remember, earlier in Activity I, we briefly discussed one main advantage of a four-chambered heart in mammals, birds, and crocodilians. A four-chambered heart allows for complete separation of the circulation of oxygenated and deoxygenated blood. This allows for a greater overall saturation of oxygen in blood supplied to the cells and tissues throughout the body. Essentially, circulation in mammals, birds, and crocodilians is separated into two separate circuits, or pathways. These pathways are the pulmonary circuit and the systemic circuit. Each of these circuits begins and ends in the heart. The pulmonary circuit involves the circulation of deoxygenated blood from the heart to the lungs for re-oxygenation, and back to the heart. The systemic circuit involves the circulation of oxygenated blood from the heart to the rest of the body, which uses up the oxygen in that blood, and the return of this deoxygenated blood to the heart.
One easy way to remember the path of blood in both the pulmonary and systemic circuits is that both circuits start in one atrium of the heart, and end in the other atrium of the heart. Each circuit is primarily associated with one side of the heart, however, because each circuit involves both the atrium and ventricle of the same side of the heart. The pulmonary circuit is associated with the right side of the heart, and involves activity of both the right atrium and right ventricle. The systemic circuit is associated with the left side of the heart, and involves activity of the left atrium and left ventricle. As you read about these pathways of blood through the heart, it may be helpful to refer to the provided heart model to visually trace the path of blood through each of these pathways.
The pulmonary circuit is the shortest of the two pathways of blood through the heart. Any time you see the word “pulmonary”, that means “relating to the lungs”. Again, the pulmonary circuit is the pathway of blood from the heart to the lungs, and back to the heart. The main function of the pulmonary circuit is to receive deoxygenated blood from the rest of the body, and deliver that blood to the lungs for re-oxygenation, before returning that blood back to the heart. On the provided heart model, locate the superior and inferior vena cava. These are two major veins that deliver deoxygenated blood back to the heart, with the superior vena cava returning deoxygenated blood from the head and upper body to the heart, and the inferior vena cava returning deoxygenated blood from the lower body to the heart. Remove the front of the heart model, and notice that both the superior vena cava and inferior vena cava empty into the right atrium. When the atria contract, this deoxygenated blood from the right atrium is pumped into the right ventricle through the tricuspid valve. Then, when the ventricles contract, the deoxygenated blood in the right ventricle is pumped up through the pulmonary semilunar valve into the pulmonary trunk, and then to the left and right pulmonary arteries, which carry blood to the lungs. In the lungs, numerous capillary beds are where oxygen diffuses from the lungs into the bloodstream (and carbon dioxide in the bloodstream diffuses into the lungs), re-oxygenating the formerly oxygen-depleted blood. See Figure 9 below for an example of these capillary beds in the lungs. After this blood is re-oxygenated, it is transported back towards the heart through the pulmonary veins, which empty into the left atrium, completing the pulmonary circuit.
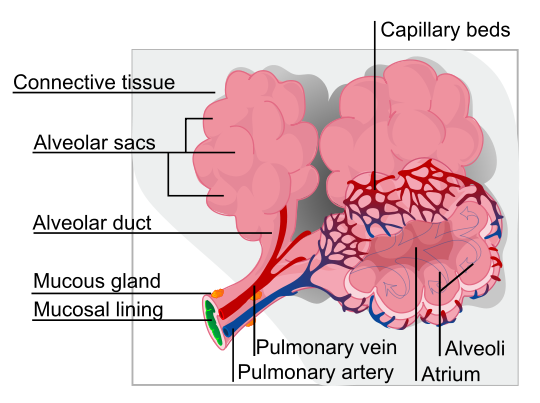
Figure 9. Illustration of alveoli (air sacs) in the lungs, and the associated capillary beds, pulmonary arteries, and pulmonary veins.
The systemic circuit is the longest of the two pathways of blood through the heart. The word “systemic” in anatomic terminology means “relating to the entire body”. Again, the systemic circuit is the pathway of blood from the heart to the entirety of the rest of the body (excluding the lungs), and back to the heart. The main function of the systemic circuit is to receive oxygenated blood from the lungs, and deliver that blood to the rest of the body, where tissues use up the oxygen in the blood, and then the return of that blood back to the heart. Again, examine the provided heart model. Remember, as previously discussed, the pulmonary circuit ends when oxygenated blood from the lungs is returned to the left atrium, marking the beginning of the systemic circuit. The systemic circuit starts with the entry of oxygenated blood into the left atrium. When the atria contract, this oxygenated blood from the left atrium is pumped through the mitral valve into the left ventricle. Then, when the ventricles contract, the oxygenated blood in the left ventricle is pumped through the aortic semilunar valve into the aorta, which eventually branches into various systemic arteries supplying blood to the rest of the body. In systemic capillaries in body tissues, oxygen diffuses from the bloodstream into those tissues. Carbon dioxide (and other wastes) from those tissues also diffuse from those tissues into the bloodstream. This blood, now depleted of oxygen is returned to the heart via systemic veins, which eventually empty into the superior vena cava or inferior vena cava, both of which empty into the right atrium of the heart, completing the systemic circuit.
The difference in the distance traveled by blood in the pulmonary and systemic circuits explains some of the anatomical differences between the left and right sides of the heart. Look at the provided heart model, and remove the anterior portion so that you can observe the chambers within. Note that the right ventricle has thinner, less muscular walls, while the left ventricle has thicker, more muscular walls. This should make sense if you consider the fact that the right ventricle, as part of the pulmonary circuit, only has to pump blood to the lungs, which isn’t very far, since the lungs are located just to either side of the heart. The left ventricle, however, as part of the systemic circuit, has to distribute blood everywhere else in the body, and thus has to work harder, thereby necessitating more muscle mass to do so.
Now that you have learned about the two pathways of blood through the heart, complete the exercise on pulmonary and systemic circulation on the worksheet at the end of this lab exercise.
ACTIVITY IV: Measures of Cardiovascular Health
Heart/cardiovascular disease is the leading cause of death in the United States, as well as the entire world. Cardiovascular disease refers to a broad range of conditions affecting the cardiovascular system, such as heart rhythm problems and congenital heart defects, but generally refers to the narrowing or blockage of blood vessels, which can lead to various other conditions, such as a heart attack or stroke. One specific example of a type of cardiovascular disease is a condition known as atherosclerosis, which is the buildup of plaque (made up of fat, cholesterol, and other substances) in the arteries, causing narrowing and hardening of the arteries, both of which reduce blood flow through those arteries (and thus blood supply to tissues). See Figure 10 below for an example of blood flow in a healthy artery, and one affected by atherosclerosis.
Figure 10. Illustration of blood flow in a healthy artery (A), and in an artery that has been narrowed by atherosclerosis (B). Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
One way in which atherosclerosis is sometimes treated is through the use of a stent, or a small mesh tube to widen narrowed arteries, or to reinforce weakened arteries. See Figure 11 on the following page for an example of the procedure used to place a stent in a narrowed artery.
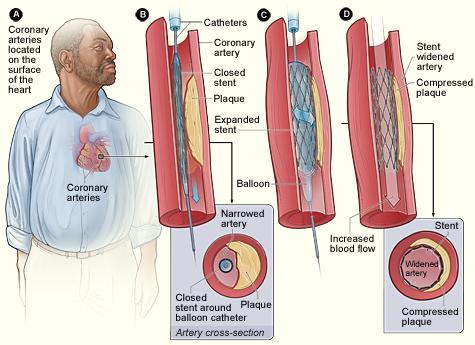
Figure 11. Illustration of the use of a stent in the treatment of an artery narrowed by atherosclerosis.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
On the exterior surface of the heart model, there are numerous coronary arteries and coronary veins. Though these were only briefly mentioned in Activity I, these blood vessels are very important, as they provide circulation to the tissues of the heart itself. Though the heart is pumping blood to the lungs and the rest of the body, the heart needs its own blood supply, as well. Since the heart is constantly pumping, it requires lots and lots of ATP to sustain that activity, and as a result, also requires a large supply of oxygen and nutrients. A blockage in one of the coronary arteries is extremely dangerous, as reduced blood supply to a region of heart tissue can result in damage or death to that tissue, resulting in a heart attack, also known as a myocardial infarction (MI). If a heart attack occurs and is not fatal, overall health is still adversely affected, as the resulting scar tissue decreases heart efficiency. Sometimes, blockages to coronary arteries can be treated using stents, as shown in Figure 10 above. However, sometimes blockages to coronary arteries are treated using a surgical procedure known as coronary bypass surgery. There are two typical approaches through which this type of surgery is performed. In one, a healthy artery in the patient’s chest is re-routed to supply blood to the heart tissue past the point of the blockage. In the other, a vein is removed from one of the patient’s legs, and grafted to the aorta and a point just past the blockage in the coronary artery. Occasionally, individuals may have blockages in multiple coronary arteries, requiring multiple bypasses. See Figure 12 for examples of each of these techniques. Look at the provided heart model showing coronary bypass surgery, and using the lab model, answer the question on the worksheet at the end of this lab exercise.
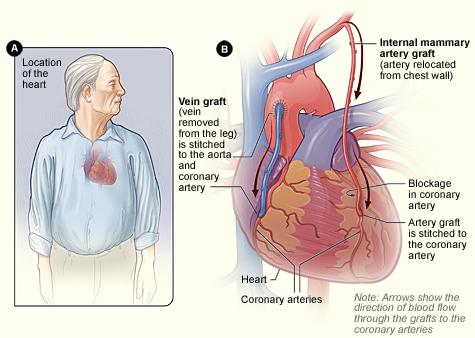
Figure 12. Illustration of the two major methods of coronary bypass surgery. Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Given the important role of the cardiovascular system, it should come as no surprise that cardiovascular health is extremely important. As a result, monitoring some aspects of cardiovascular function is part of almost every routine medical examination. During such examinations, an idea of cardiovascular health can be determined by listening to the heart for any abnormal sounds, and determination of heart rate and blood pressure. In this activity, you will be measuring your own heart rate (pulse rate) and blood pressure. The provided stethoscopes can also be used for you and your partner to listen to one another’s hearts, as well.
The resting heart rate of most healthy individuals typically falls within the range of 60 to 100 beats per minute (bpm). However, in extremely active or athletic individuals, resting heart rate may be as low as 40 bpm. Typically, lower resting heart rates reflect greater cardiovascular health. To measure your own heart rate, take the first two fingers of either hand (not the thumb), and lightly press over the radial artery (on the thumb side of the inside of your wrist). Count the number of pulses you feel during a period of 30 seconds, and multiply that number by 2. The resulting number is your heart rate in bpm. Record your heart rate on the worksheet at the end of this exercise.
To maintain good cardiovascular health, aerobic exercise, or exercise that strengthens the heart and lungs. During aerobic exercise, a target heart rate of approximately 50-85% of your estimated maximum heart rate is generally suggested. To estimate your maximum heart rate, subtract your age from 220. Then multiply the resulting number by 0.5. The result would be a good minimum target heart rate during moderate aerobic exercise. Next, multiply your estimated maximum heart rate by 0.85. The result would be a maximum target heart rate during intense aerobic exercise. Record your estimated maximum heart rate and target heart rate range on the worksheet at the end of this exercise. Optionally, your instructor may ask you to exercise (jumping jacks or running in place) for a few minutes, and then have you record your heart rate immediately after exercise. If your instructor asks you to do this, record your heart rate after exercise in the worksheet at the end of this exercise, as well.
Another measure of cardiovascular health is your blood pressure. Blood pressure is defined as the pressure, or force, of blood pressing against the walls of blood vessels. Of course, this force is ultimately the result of the pumping action of the heart, so monitoring blood pressure is a good way of monitoring overall cardiovascular health. Blood pressure readings actually consist of two numbers. The first number in a blood pressure reading is always the largest number, and the second number is smaller. The larger number is called the systolic pressure, which is the pressure of blood in an artery during the peak of systole, or contraction of the ventricles of the heart. The second, smaller number is called the diastolic pressure, which is the pressure of blood in an artery during the peak of diastole, or relaxation of the ventricles of the heart. It should make sense that the systolic pressure is always greater, since the systolic pressure is the pressure of blood when the heart is actively contracting, creating greater pressure in the arteries. Blood pressure readings are usually reported visually in a format such as “120/80”, where the number before the slash is the systolic pressure, and the number after the slash is the diastolic pressure. When reported verbally, the previous blood pressure would be reported as “120 over 80”.
Normal blood pressure is considered to be values less than 120/80. Regular monitoring of blood pressure is important, as hypertension (high blood pressure) substantially increases an individual’s risk of various other health complications, such as heart attack, stroke, kidney damage, damage to the retina of the eyes, erectile dysfunction in men, and even dementia/Alzheimer’s disease. High blood pressure often has no noticeable symptoms itself, but is often referred to as the “silent killer”, due to the increased risk of death due to heart attack, stroke, or kidney disease associated with hypertension. Table 1 below shows the American Heart Association’s newest guidelines on classifying blood pressure values. Patients with hypertension are typically treated with medications to keep blood pressure within lower, safer ranges, but lifestyle changes (such as smokers quitting smoking, reduction of sodium and saturated fats in the diet, weight loss, aerobic exercise, and reduction of alcohol consumption are usually also recommended to prevent further worsening of hypertension
Table 1. New (2017) blood pressure categories from the American Heart Association
|
Category |
Blood Pressure Values |
|
Normal |
Less than 120/80 |
|
Elevated |
Systolic between 120-129 and diastolic less than 80 |
|
Stage 1 hypertension |
Systolic between 130-139 or diastolic between 80-89 |
|
Stage 2 hypertension |
Systolic at least 140 or diastolic at least 90 mm Hg |
|
Hypertensive crisis |
Systolic over 180 and/or diastolic over 120 |
The traditional method of measuring blood pressure is through the use of a stethoscope and a device called a sphygmomanometer, which consists of an inflatable cuff attached by rubber tubing to an inflator bulb and a pressure gauge. To obtain a blood pressure reading using a sphygmomanometer, the cuff of the sphygmomanometer is placed around the upper arm, right above the bend of the elbow. At this location, the blood pressure reading obtained is a measurement of the pressure of blood in the brachial artery (refer back to Figure 8). The cuff is then inflated to a pressure that is high enough to cut off blood flow beyond the cuff. A stethoscope is then used to listen at a location just below the cuff, and the person taking the reading slowly begins releasing the pressure in the cuff, while simultaneously continuing to listen while also visually monitoring the pressure gauge on the sphygmomanometer. What the person taking the reading is listening for are some special sounds called the sounds of Korotkoff, which indicate changes in blood flow in the artery. When the pressure in the cuff is greater than the systolic pressure in the artery, there is no blood flow past the cuff, and no sounds are heard. As the pressure is decreased, when the pressure in the cuff is equal to the systolic pressure, a slight knocking sound should be heard as blood begins to flow past the cuff, and the pressure on the gauge when the knocking sound is heard is recorded as the systolic pressure. As the pressure is continually decreased, continued knocking or turbulent sounds are heard, because even though blood is flowing past the cuff, the artery is still somewhat compressed. However, eventually, when the pressure in the cuff is equal to the diastolic pressure in the artery, all sounds should stop, as the artery is no longer compressed, and blood is flowing completely freely through the artery. The pressure at which all sounds stop is then recorded as the diastolic pressure. It is fairly difficult to take your own blood pressure using this method, so you and your lab partner should attempt to get a blood pressure reading on one another. Ideally, blood pressure readings should be taken when an individual is seated, with legs uncrossed, and supporting the arm in which the blood pressure is being taken. To get a blood pressure reading from your partner, follow the instructions below.
- Clean the eartips of your stethoscope using the provided alcohol swabs.
- Place the eartips of your stethoscope in your ears, making sure that they are pointing forward (away from you), and that they form a tight seal inside your ears. You should be able to hear very little in the room around you if you are using the stethoscope properly.
- Have your partner present you with the arm of their choice. Blood pressure readings can be taken from either arm. If they are wearing long sleeve shirts that are thicker than an average T-shirt, their sleeve should be pushed up well past their elbow.
- Place the cuff of the sphygmomanometer around your partner’s upper arm, making sure to line up the arrow on the cuff with the location of the artery in their arm.
- Using the inflator bulb, rapidly inflate the pressure in the cuff to about 180 mmHg.
- Place the edge diaphragm or bell of your stethoscope just right under the bottom edge of the cuff, and listen. Initially, you should hear no sound, since blood flow past the cuff is completely obstructed.
- While continuing to listen, begin slowly releasing the pressure on the cuff by slightly unscrewing the valve at the end of the inflator bulb. Make sure you are also visually monitoring the pressure gauge on the cuff the entire time.
- Continue to listen as the pressure decreases, and as soon as you hear a clicking or popping noise, note the pressure on the gauge and record this as your partner’s systolic pressure.
- Continue to allow the pressure to decrease as you continue to listen and monitor the pressure gauge. As soon as any sounds you hear stop, note the pressure on the gauge and record this as your partner’s diastolic pressure.
- Remove the cuff from your partner’s arm, and the stethoscope from your ears, and again clean the eartips of the stethoscope with alcohol swabs.
- After attempting to get a blood pressure reading from your partner, swap places and allow them to attempt to get your blood pressure using all the steps above.
It can be tricky to train your ear to listen for the sounds of Korotkoff to obtain a blood pressure reading using the traditional method listed above, but try the traditional method of obtaining a blood pressure reading from your partner at least once. If you have difficulty listening for the sounds of Korotkoff, you can try the traditional method a second time, or you can use one of the provided electronic blood pressure cuffs in lab to get a reading of your own blood pressure. On the worksheet at the end of this lab exercise, record your own blood pressure (not your partner’s). Several factors can elevate your blood pressure above your actual baseline blood pressure. Blood pressure readings should be taken when you are quiet, relaxed, and comfortable. Several factors may falsely elevate blood pressure beyond your normal baseline, such as talking during the reading, recent previous activity, recent caffeine consumption, recent tobacco use, anxiety, a full bladder, feeling chilly, etc.

Figure 13. Measuring blood pressure using a stethoscope and sphygmomanometer. Credit: Elmien Woolvardt Ellison. Obtained from http://openi.nlm.nih.gov/, licensed under https://creativecommons.org/licenses/by/2.0/
BI 102 Lab Worksheet: Cardiovascular Name ___________________________ Section _______
ACTIVITY I: Anatomy of the Heart
Using the available human heart models, write the number on the model beside each appropriate structure listed below:
_____ Aorta/aortic arch
_____ Aortic semilunar valve
_____ Inferior vena cava
_____ Left atrium
_____ Left pulmonary artery
_____ Left pulmonary veins
_____ Left ventricle
_____ Biscuspid (mitral/left AV) valve
_____ Pulmonary semilunar valve
_____ Pulmonary trunk
_____ Right atrium
_____ Right pulmonary artery
_____ Right pulmonary veins
_____ Right ventricle
_____ Superior vena cava
_____ Tricuspid (right AV) valve
ACTIVITY II: Anatomy of Blood Vessels
Match the descriptions below to the correct blood vessels.
| _____ Blood vessels from heart to the neck and head | A. aorta |
| _____ Blood vessels to heart from the neck and head |
B. brachial arteries |
| _____ Blood vessels from heart to the lungs for oxygenation | C. carotid arteries |
| _____ Blood vessels to heart from the lungs | D. inferior vena cava |
| _____ Blood vessel to heart from the head, arms, & upper body | E. pulmonary veins |
| _____ Blood vessel to heart from the lower/middle body | F. pulmonary arteries |
| _____ Largest artery in body from heart to many body regions | G. renal arteries |
| _____ Blood vessels from heart to the upper arm; blood pressure is taken here | H. renal veins |
| _____ Blood vessels from heart to the kidneys | I. superior vena cava |
| _____ Blood vessels to heart from the kidneys | J. jugular veins |
ACTIVITY III: Pulmonary and Systemic Circulation
In the diagram, label the left atrium (LA), right atrium (RA), left ventricle (LV), right ventricle (RV), aorta (A), superior vena cava (SVC), inferior vena cava (IVC), pulmonary trunk (PT), left pulmonary artery (LPA), right pulmonary artery (RPA), left pulmonary veins (LPV), right pulmonary veins (RPV), mitral valve (MV), tricuspid valve (TV), aortic valve (AV), and pulmonary valve (PV).
Using colored pencils (blue to represent deoxygenated blood, and red to represent oxygenated blood), draw colored arrows to show the direction of blood flow through all of the labeled structures. Make sure that you have arrows showing blood flow drawn in all blood vessels shown.
| From Venae Cavae | From lungs |
| –> | –> |
| –> valve | –> |
| –> | –> valve |
| –> valve | –> |
| –> | –> valve |
| –> | –> To Aorta |
| –> To lungs |
Correctly trace the path of blood flow through the heart from the vena cavae to the aorta. Use each of the terms only once: Aortic semilunar, Bicuspid (AV), Left Atrium, Left Ventricle, Pulmonary arteries, Pulmonary semilunar, Pulmonary trunk, Pulmonary veins, Right Atrium, Right Ventricle, Tricuspid (AV)
| From Venae Cavae | From lungs |
| –> 1. | –> 7. |
| –> 2. valve | –> 8. |
| –> 3. | –> 9. valve |
| –> 4. valve | –> 10. |
| –> 5. | –> 11. valve |
| –> 6. | –> To Aorta |
| –> To lungs |
ACTIVITY IV: Measures of Cardiovascular Health
Examine the heart model in lab showing coronary bypass surgery, and fill in the blank below:
The coronary bypass model in lab has ____ (number of) bypasses.
Your resting heart rate: ____ bpm OPTIONAL: Your heart rate after exercise: ____ bpm
Your estimated maximum heart rate (220 – your age): ____ bpm
Your target heart range during exercise (50-85% max): between ____ and ____ bpm
Why does heart rate increase during aerobic exercise?
Your blood pressure: ____/____How would your blood pressure be classified using the AHA’s guidelines?